Last month, Barbara Pfeiffer had surgery to remove both her breasts. A year ago, she had a total hysterectomy, removing her uterus and ovaries. The 46-year-old has never been diagnosed with cancer.
She had these healthy body parts surgically removed because she has a strong family history of cancer and a genetic mutation making it overwhelmingly likely that she would develop breast or ovarian cancer in her lifetime.
She learned she has the BRCA 1 gene mutation, which is far more common among Ashkenazi Jews than in the general population, while her mother was dying from breast cancer that had spread.
“I looked at how aggressive my mom’s cancer was. I thought ‘I can’t like any body part so much that I would let it kill me,’” said Pfeiffer, a marketing consultant who lives in Hoboken, N.J. “It was worth it not to go through what she did.”
Pfeiffer is one of a growing number of Ashkenazi Jewish women who learn that they have a mutation on the BRCA 1 or BRCA 2 genes (pronounced “bracka”), and though they have never been diagnosed with cancer, are having their breasts, ovaries and uteruses removed in an effort to reduce their risk.
The risk of these cancers is as high as 85 percent for women with these mutations. They are also prone to developing cancer at a younger age, when the disease can be more aggressive. Without the mutation, American women have a 13 percent chance of having breast cancer in their lifetime. BRCA gene mutations are also found in the general population, affecting 1 in 450 women. The mutation is 10 times more common in Ashkenazi women, affecting 1 in 40.
Women carrying the BRCA defects also have a 30 percent to 50 percent risk of developing ovarian cancer, one of the deadliest cancers, compared to 2 percent of women without it.
While the BRCA mutations were discovered about a decade ago, and women have been having breasts and reproductive organs removed prophylactically for some time, awareness of genetic testing is growing, experts say. As a result, so is the number of surgeries. And as surgical breast reconstruction techniques improve, it makes it easier for women to contemplate having preventive mastectomies, say some who have made the difficult decision.
Dr. Ariela Noy, who carries the BRCA 2 mutation, had a double mastectomy and a complete hysterectomy in back-to-back surgeries last summer, when she was 41. Losing her ovaries was the most difficult part emotionally, she said. “Was I still going to feel female? The issues of being surgically put into menopause were huge, just overwhelming. I was terrified.”
Fortunately, as a mother of three, she already had the family she wanted. Unlike most women who discover they have the gene mutations, Noy, an oncologist at Memorial Sloan Kettering Cancer Center on the Upper East Side, had no family history of breast cancer, though she has no female relatives besides her mother. The Nazis killed most female relatives of the grandfather who she believes passed the trait to her, she says. “We don’t know what our family histories would have been” had her relatives not been slaughtered in the Holocaust.
Most people, if not diagnosed with cancer, pursue genetic testing because they have multiple direct blood relatives who had breast or ovarian cancer.
Pfeiffer’s maternal grandmother died of breast cancer at 36, and her aunt at 37. Her mother died last October after battling the disease for 15 years.
“We always said we were just one of those families that’s going to get breast cancer, and I never realized there was genetic testing available,” said Pfeiffer, who is recovering from her surgery at home after having her mastectomy and the first of two surgeries for breast reconstruction.
She only learned about it a year and a half ago, after a new gynecologist sent her for high-risk screening. They found that she had the BRCA-1 mutation, as did her mother.
“It validated something that I’d thought all along, and almost made me feel a bit better,” Pfeiffer says. “Now I felt like I have some control over it.” Pfeiffer and her husband decided not to have children long before she learned of the mutation.
After meeting with a genetic counselor, who laid out the options available to women with the BRCA mutations – close surveillance, with MRIs, sonograms and mammograms; surgical removal of the ovaries and uterus; or surgical removal of them plus the breasts – she decided to take the most aggressive route.
“For me, it was a matter of when I’d get cancer, not if,” she said.
And while these surgeries do not eradicate a woman’s risk of getting these cancers, it does reduce it by about 90 percent.
While widely considered a woman’s disease, breast cancer and these genetic mutations can also affect men.
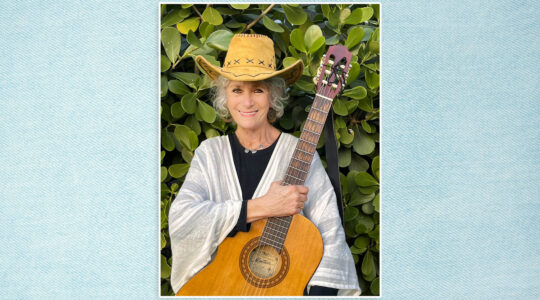
Debra Stepen, a psychotherapist in Los Angeles, had a prophylactic mastectomy in June. She moved quickly after learning that she had the genetic mutation. She was supposed to have the blood test done in February, but postponed it because she was sitting shiva for her father, who had just died of breast cancer. She plans to have the second stage of her breast reconstruction in September – “right before yontiff,” she says. “This year, we’re catering.” She expects to have a hysterectomy at the end of the year.
Stepen, who is 51, says she feels relief that her breasts have been removed. She describes them as “ticking time bombs.”
Genetic Legacy
The genetic legacy of the BRCA mutations is difficult to confront.
Noy’s children are young — her daughter is 10 and her sons are 12 and 14. “They know I had preventative surgery,” she says. “I explained it to them like it was a vaccine and they accepted that, though they knew what body parts were involved.”
She is not sure when she will tell them that they may have inherited the BRCA 2 mutation.
“I don’t think they have to live their childhoods knowing about this,” she said. “I feel blessed that I didn’t know about this until I was 41, and had my children. Do I tell them when they’re 25? I don’t know. My children will make their own decisions about getting tested” once they’re adults, she says.
Still, unanswered questions weigh on her.
“If she has it, does it mean that my daughter should have her children earlier” than she might have otherwise? asked Dr. Noy, referring to the fact that the incidence of these cancers rises with age. “I hope that she doesn’t feel her biological clock is ticking faster than the average person,” she said.
Stepen is Orthodox and, while many of the considerations relating to these surgeries are common to everyone, some are specific to being part of the religious community.
She has three adult stepchildren. But for women who have biological children, knowing that each has a 50-50 chance of inheriting the genetic mutation can become a heavy burden. In the Orthodox community a family history of genetic disorders can become an obstacle to getting married.
Elsa Reich is a genetic counselor at the New York University School of Medicine, and sees a lot of women contemplating testing for these mutations.
“It has been difficult for many of my religious patients to have genetic testing, and if they do it’s not uncommon for them not to tell other members of their family,” she said. “I know of several women who have been tested, and been positive for the genes, but they don’t have surgery because they don’t want outward signs” that could lead to questions about why they had their breasts removed.
Even when diagnosed with breast cancer, “I know many who have not told their families, and they frequently don’t tell their children,” said Reich, citing a combination of concern about their children’s ability to get married and not wanting to raise the anxiety level of the whole family.
Some also consider Jewish legal issues. Rabbi Moshe Tendler, a leading Orthodox medical ethicist, says he has been asked “many times” for a religious opinion about whether it is possible to cut out healthy tissue in these cases.
It is a difficult topic, he says. While there is a Jewish legal imperative to protect life, it intersects here with the injunction against harming one’s own body.
“No one can fault a woman for running scared and doing these surgeries,” he said. “But it isn’t a 100 percent guarantee” that she won’t get these cancers, he noted, and he recommends against them, preferring instead that women increase their surveillance with non-invasive tests. With growing knowledge of genetics these challenging issues arise with increasing frequency, he said. “It’s a reaffirmation that we are individuals dependent upon God’s grace, and that we cannot guarantee against the angel of death.”
Resources: FacingOurRisk.org, an online network and information resource for women with hereditary breast and ovarian cancer issues.
Sharsheret.org, a network for pre-menopausal Jewish women confronting breast cancer.
The New York Jewish Week brings you the stories behind the headlines, keeping you connected to Jewish life in New York. Help sustain the reporting you trust by donating today.