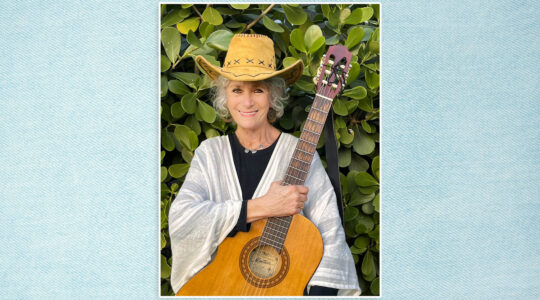
Jerusalem — Linda Gradstein has a strong family history of breast cancer. Her mother survived breast cancer in her 60s but died a decade later from leukemia. Her maternal grandmother died of the disease in her 50s and her father’s father died of it in his 60s.
So when Gradstein’s physician suggested she get tested for the BRCA1 & 2 mutations that greatly raise the risk of developing breast and ovarian cancers especially in Ashkenazi women, the 57-year-old Jerusalem resident readily agreed.
When the test came back negative “I felt quite relieved, as if I didn’t have to deal with this now,” Gradstein, a journalist, told The Jewish Week.
Even so, Gradstein is aware that she may harbor another type of breast cancer-inducing gene mutation.
“It’s scary because I feel I have no control over it. I try not to think about it too much,” she acknowledged.
Hoping to lower her risk, Gradstein eats healthily and exercises regularly, especially because being overweight is a risk factor for breast cancer. She also continues to get mammograms, may retest for the BRCA1 & 2 mutations (the test has improved over time), and is considering undergoing testing for other gene mutations.
Gradstein is one of the many women who have tested negative for the BRCA1 & 2 mutations but are still considered to be at higher than average risk of developing breast cancer.
Just 5 to 10 percent of breast cancers are thought to be hereditary, caused by mutated genes inherited from a parent. But these low odds are of little comfort to families where multiple relatives have been diagnosed, especially prior to the onset of menopause.
BRCA1 and 2 mutations account for an estimated 20 to 25 percent of hereditary breast cancers and about 5 to 10 percent of all breast cancers.
Li-Fraumeni and Cowden syndromes raise the risk of developing several types of cancer, including breast cancer. Additionally, “more than 150” other genetic mutations have been associated with a slightly higher breast cancer risk, according to a report by the American Cancer Society.
A mutated gene can be inherited from a person’s father or mother.
Physicians advise high-risk BRCA-negative women to undergo frequent breast exams that combine a physical exam by a breast specialist with mammograms and/or ultrasounds. Some also advise an MRI, in between mammograms.
“Otherwise, you have almost a year with no imaging,” said Dr. Tal Hadar, a breast surgeon at Shaare Zedek Medical Center, who advises many of her patients at risk for hereditary breast cancer to alternate mammograms with MRIs every six months, along with a clinical exam.
A trained breast specialist may be able to detect breast lumps and spot irregular discharge from the nipples that imaging technology can miss.
Professor Tamar Peretz, who heads Hadassah’s Sharett Institute of Oncology, Center for Malignant Breast Diseases, emphasized that not every woman who has a mutated gene will develop breast cancer.
“We cannot say or define exactly why one woman with a mutated gene develops cancer and her sister with the same genomic profile does not. This is part of our research,” Peretz said.
“But there is data suggesting that a healthy lifestyle can reduce the likelihood of developing breast cancer.”
Factors such as hormone exposure, environmental exposures, diet, exercise and other genes can affect cancer risk, both in people with inherited genetic mutations that increase cancer risk and people who do not have a mutation.
Based on a woman’s estimated risk and her personal preferences, her physician may recommend comprehensive panel testing (testing for a number of gene mutations) to determine whether she has a non-BRCA mutation that could raise her breast cancer risk.
Although limited testing for just a handful of so-called Ashkenazi mutations, including BRCA1 & 2, was once the norm, some cancer specialists now advise their patients to opt for “full sequence” testing, with searches for those mutations plus many others.
“We know if a woman is Ashkenazi and tested [negative] only for the mutations most common in Ashkenazi Jews, there is still a 4-to-5 percent probability she is carrying another mutation in the BRCA gene,” Peretz said. And among the BRCA-negatives, there are several gene mutations in other genes that have already been identified.
Before opting for genetic testing a woman should sit with a genetic counselor not only to gauge her risk based on everything from family history to whether she breastfed her children, but to discuss the implications of discovering a non-BRCA mutation.
While the risks of having certain mutations (such as PALB2, CHEK2, ATM, BARD1, PTEN, TP53, NF1, CDH1, NBN, and STK11) are well-established, there are many other mutations whose level of risk is not currently known.
“There are instances when the tests come back with variants of uncertain significance, which means that there is a mutation but its potential impact on health is unknown at this time,” said Dr. Ephrat Levy-Lahad, the director of the Medical Genetics Institute at Shaare Zedek Medical Center in Jerusalem.
While scientists may one day learn more about the mutation’s implications, right now geneticists cannot say how much risk the mutation carries. Not everyone is comfortable living with that uncertainty.
When a mutation’s implications are known, knowing you are carrying that variation may lead to more positive outcomes, according to Hadar.
Speaking at a medical gathering, Hadar noted that patients at Shaare Zedek’s Noga clinic for women who are BRCA1 & 2 positive “are usually diagnosed earlier [than patients who are not BRCA-positive] because they are aware of the danger and have a better prognosis.” They have more frequent screenings and may decide to have a preventative double mastectomy to prevent cancer from developing.
Being BRCA1 & 2 negative has only boosted Gradstein’s desire to learn as much as possible about her cancer risk.
“I feel like if we have the opportunity to have more information, why wouldn’t we want to have it, in the hopes of early detection?” she said.
The New York Jewish Week brings you the stories behind the headlines, keeping you connected to Jewish life in New York. Help sustain the reporting you trust by donating today.