(JTA) — For the second year, COVID-19 has made it so Jews who want to attend High Holidays services must undergo a complicated risk calculation.
Is it safe to go to synagogue for Rosh Hashanah and Yom Kippur? Should I bring my children? Is the shofar — the horn whose blasts punctuate the holy days — a potential vector of disease?
Last year, five months into the global pandemic that has killed more than 4.5 million people globally, the answers were fairly straightforward, if dispiriting: Stay home, or at least stay masked and very far apart. Anyone could be carrying the disease, and anyone could catch it.
This year, the situation is more complex. Most American adults have been vaccinated, with the uptake of vaccination among Jews among the highest of any religious group, but children under 12 aren’t eligible for vaccination. For a small but vociferous segment of Americans, grudging acceptance of masking last year has morphed into antipathy this year.
Meanwhile, the highly transmissible Delta variant, alongside evidence of potentially waning protection from vaccines and emerging data showing that even vaccinated people can catch and transmit COVID-19, further complicate the picture.
“This is going to be a personal decision that will be dependent upon many factors,” said Dr. Aaron Glatt, a rabbi and epidemiologist who has spent the pandemic making medical information accessible to others in his Orthodox community in suburban New York.
“What type of shul you will be going into, the incidence of vaccination in that shul, the incidence of risk factors in your personal family — is everybody vaccinated? If they are, are they high risk? There are a tremendous number of variables,” said Glatt, who is the chief of infectious diseases and hospital epidemiologist at Mount Sinai South Nassau on Long Island and an assistant rabbi at the Young Israel of Woodmere.
He added, “And it also depends on the level of risk that people are willing to take with all those variables taken into account.”
So what is a Jew supposed to do? We’ve answered a few of the most frequently asked questions about how to observe High Holidays during the coronavirus pandemic, round two.
Is it safe to travel for Rosh Hashanah, or to have someone travel to me?
The appeal of getting far-flung family members together to share the holiday is undeniable. And we’ve learned a lot about how to manage risk during pandemic travel. So jumping on a plane may feel like a better idea this year than last year.
But there are some caveats: Someone who is vaccinated and heads to visit people who are vaccinated in an area with a high vaccination rate is at less risk than if one party isn’t vaccinated or even if both are, but there is a high level of community transmission.
Glatt advises people considering traveling to consider “where you’re traveling to [and] the incidence of COVID in that area.” In some parts of the country, especially in the South, hospitals are near or even over capacity amid the Delta-fueled surge. They may not be safe destinations when it comes to COVID-19 or any other health issue that can arise while traveling.
The Centers for Disease Control is advising Americans to delay travel until fully vaccinated, and even then to wear a mask while in shared transportation. Unvaccinated travelers, including children, are urged to test before and after traveling and stay away from especially vulnerable people upon their return.
Is it safe to attend synagogue for Rosh Hashanah and Yom Kippur?

Here, again, context matters, and so does one’s own risk tolerance. In a community where transmission is high and vaccination rates are relatively low, the risk from praying together in person is going to be higher than in a community where most people are vaccinated and there are relatively few cases.
People who are unvaccinated are always at more risk than people who have been fully vaccinated: They are much more likely to require hospitalization or to die after catching COVID-19.
The synagogues you’re considering attending almost certainly have policies in place that you can assess. You can also ask them for more information before deciding whether to attend.
- What is their policy on masking? A mask requirement offers a low-cost, low-effort safeguard against transmission. It is also a good signifier of a conservative approach to safety.
- Are vaccinations required for eligible people? Some synagogues are strongly urging vaccinations, while others are requiring them for everyone over 12. Some are even requiring attendees to prove their vaccination by sharing their vaccine card ahead of time or at the door. (In some places, including Florida, requiring vaccination or asking for evidence of vaccination is illegal.)
- Is any prayer taking place outdoors? Some synagogues are moving as much of their services as possible outside, to open-sided tents where transmission is less likely. Glatt says all communities should strive to offer some outdoor options for people who feel more comfortable there.
- How well does air circulate? Since last year, it’s become clearer that good ventilation is an important factor in preventing the spread of disease. Synagogues that have good airflow will offer safer experiences than synagogues with poor air circulation.
Many Jewish communities, especially Orthodox ones, are home to a wide range of perspectives on whether masking and distancing should be required at this stage of the pandemic. Glatt says synagogues should be advocating vaccination, calling that “the correct medical and halachic recommendation,” referring to Jewish law. But he also says he believes that synagogues can safely accommodate people with a wide range of approaches to COVID-19.
“There should be areas where people who are vaccinated and are concerned should be able to daven [pray] with a mask on, and everybody in that area should have a mask on,” he said. “At the same time, I have not made the recommendation that everybody should be masked in every situation at every shul. I think there are people who might be uncomfortable with that for various reasons and we need to try to accommodate them as well.”
Should children under 12 go to High Holiday services this year?
Children under 12 are not yet eligible for vaccination in the United States; government approval for a vaccine for kids is expected sometime before the end of the year. That means the children’s services that most synagogues hold on the High Holidays are effectively for unvaccinated people only, at a time when the Delta variant has elevated pediatric hospital admissions to pandemic-high levels. It also means that including children in adult services reduces the proportion of vaccinated people in the room.
Glatt described the question of whether and how to include children as one that is concerning, with no one-size-fits-all answer.
“I think that’s a decision that every shul has to make, how they wish to handle that. If you’re dealing with an elderly population, to have them sitting next to younger children that aren’t vaccinated and their mask wearing is of some concern… I think that needs to be addressed,” he said. “If you’re dealing mostly with a younger population, they’re vaccinated mostly, they’re willing to take the chance — that may be a different situation. It’s a concern.”
Many synagogues are holding their children’s services outside to mitigate risk. But not every synagogue has that option, and in some communities, that may not be everyone’s preference. It also could be uncomfortably hot in much of the South at the beginning of September.
Glatt says parents should take appropriate precautions, but he notes that many children are in communal settings already by attending school, which conveys an equivalent level of risk. (Tens of thousands of children nationwide have already spent time in quarantine this school year because of in-school exposures to COVID-19.)
“I do think children should be in shul,” Glatt said. “If this was the only situation where they were being exposed, that might be a different story. But they’re getting together anyway.”
Is it safe to blow the shofar in an indoor space?
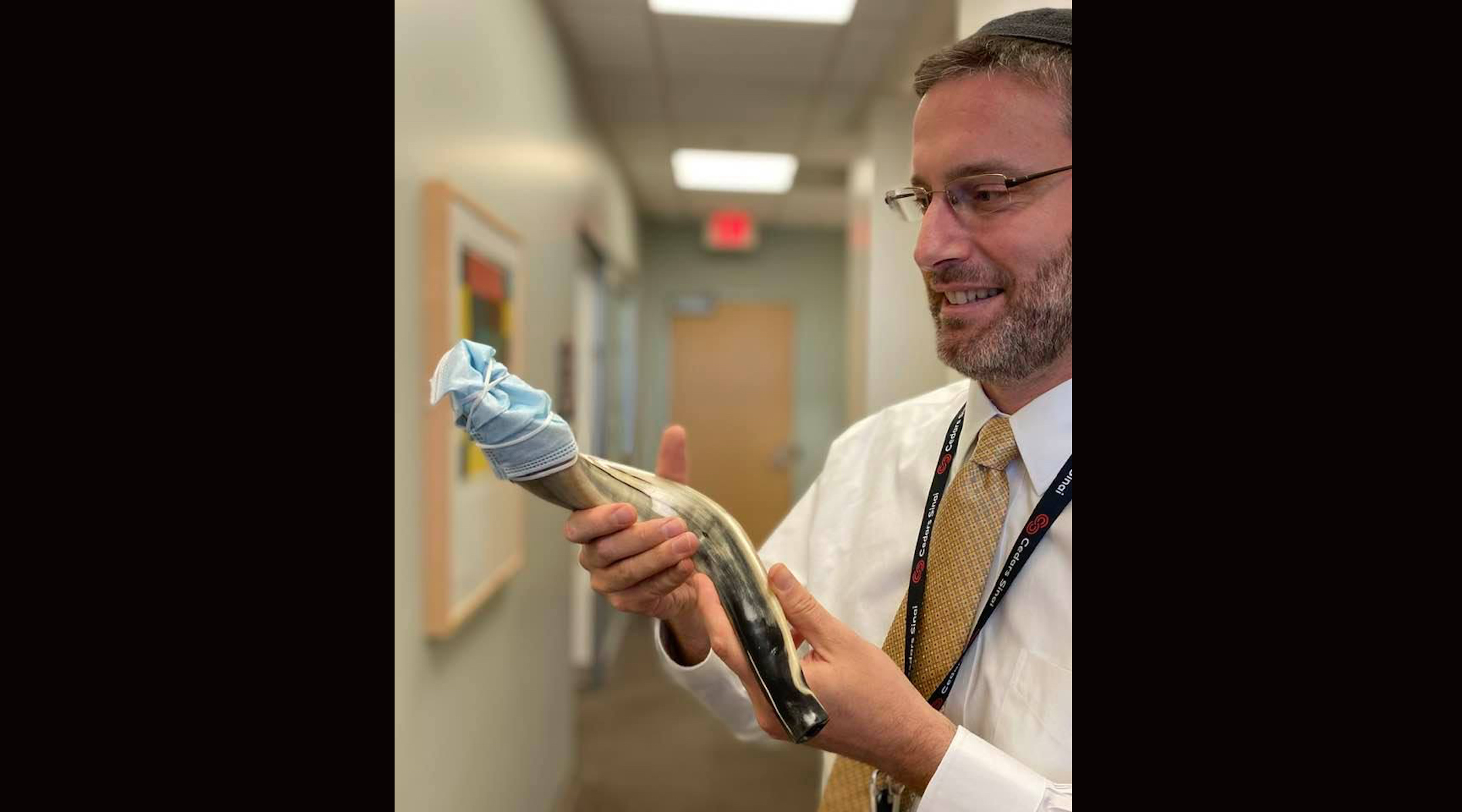
Rabbi Jason Weiner announced in July 2020 that he planned to put a mask on his shofar during the High Holiday season, a choice that many others later made to ensure that they do not spread the coronavirus when blowing the ram’s horn. (Courtesy of Weiner)
Images of people blowing shofars with surgical masks over their openings became a visual trademark of last year’s High Holidays. This year, vaccines and widely available COVID-19 testing mean it’s relatively straightforward to ensure that the shofar does not spread disease.
“If the person blowing the shofar is vaccinated and asymptomatic, that should be fine. Let it blow, possibly not right next to everybody else,” Glatt said, noting that the person should also have no known virus exposures.
Some synagogues are bringing their congregations outside to hear the shofar at the end of the service, rather than during it. To play it extra safe, others are requiring a negative PCR test — the more reliable type of test on the market — for shofar blowers in the days before the holiday.
What should I do if I find out someone at my services had COVID-19?
That’s a realistic concern. If Rosh Hashanah were today, the virus is so prevalent in the United States that in some places, there would be nearly a 100% chance that someone in the room would have COVID-19 for any event of 100 people, a typical size for smaller-than-usual services. That includes almost all counties in Florida, currently the hardest-hit state, according to an online “COVID-19 Event Risk Assessment Planning Tool” produced by a team of researchers.
The CDC has clear guidelines about what to do if you’re exposed to COVID-19 — which it says happens if you’ve spent more than 15 minutes total over a 24 hour period near someone with the virus. You should get tested 3-5 days after the exposure and wear a mask when you are around other people until you get a negative result. If you get a positive result, you should isolate for 10 days, even if you don’t develop symptoms.
In the early days of the pandemic, worship services were identified as key vectors of disease in both the United States and Israel, in part because some people continued to attend them after reducing other contacts and in part because of the kinds of activities — including singing — that typically happens at them. So following post-exposure recommendations could be key to making sure that High Holiday services don’t become spreading events.
What if you find out that the person who had COVID-19 was all the way on the other side of the room during services? Does that count as an exposure? Glatt’s answer points to the uncertainty that’s swirling as the Jewish world prepares to enter 5782.
“I don’t think so,” he said. “But it’s really unknown.”
Shira Hanau contributed reporting.
JTA has documented Jewish history in real-time for over a century. Keep our journalism strong by joining us in supporting independent, award-winning reporting.






